Understanding EHR Systems: Definition and Overview

In the realm of modern healthcare, the transition from traditional paper-based medical records to electronic health records (EHRs) marks a significant advancement. The adoption of EHR software offers numerous benefits, yet it also presents challenges that healthcare providers must address. This article delves into the definition, benefits, problems, and examples of EHR systems, offering insights into their development and implementation.
Defining EHR, EMR, and PHR
Electronic health records (EHRs), electronic medical records (EMRs), and personal health records (PHRs) serve similar purposes but differ in scope and functionality.
Electronic Medical Records (EMRs)
EMRs are digital versions of patients’ paper charts, containing medical histories and clinical data accessible within a single practice. While EMRs streamline charting and data tracking, they are primarily confined to the originating medical office.
Electronic Health Records (EHRs)
EHRs encompass a broader perspective, focusing on the comprehensive health journey of patients across multiple healthcare providers. EHRs facilitate data sharing between practices, allowing seamless transitions of patient records across different settings, including labs, pharmacies, and emergency rooms.
Personal Health Records (PHRs)
PHRs empower patients to manage and update their health information independently. Patients can compile various data, such as lab results and medical histories, into a single repository, promoting active engagement in healthcare management.
Benefits of EHR Systems
EHR systems offer numerous advantages over traditional paper-based records, including:
- Enhanced data accessibility and sharing
- Reduction of duplicate testing and medical errors
- Promotion of patient participation in healthcare decisions
- Improvement of care coordination among providers
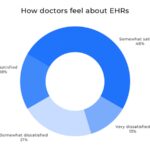
Challenges and Barriers
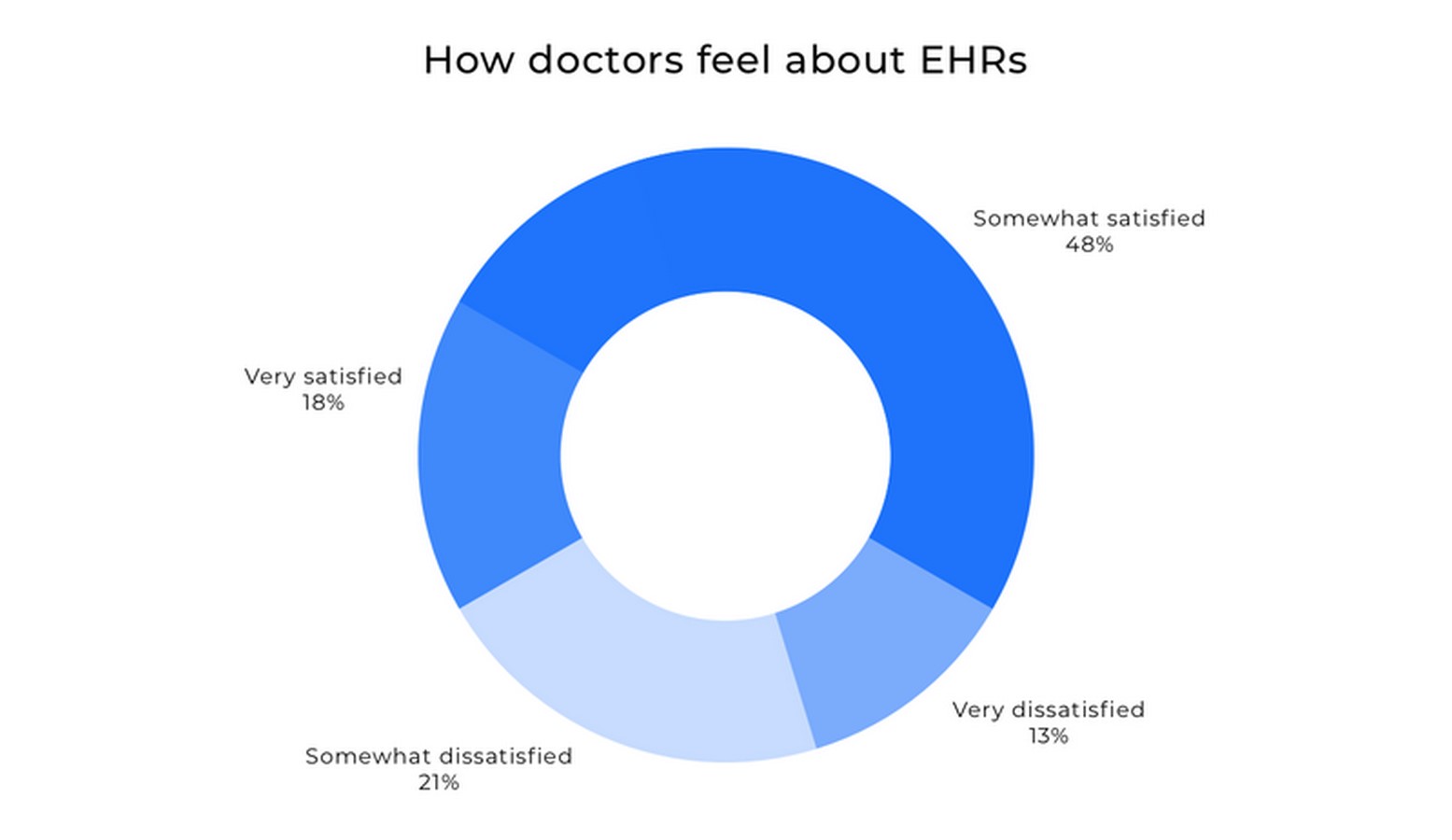
Despite their benefits, EHR systems present challenges and barriers to adoption, particularly among healthcare providers. Common issues include:
- Time Consumption: Physicians spend significant time navigating EHR systems, leading to decreased efficiency and increased burnout.
- Limited Clinical Utility: Some doctors perceive EHRs as data storage tools rather than valuable clinical assets, highlighting the need for enhanced functionality.
- Poor User Interface: Inefficient design elements contribute to user frustration and increased screen time, underscoring the importance of intuitive interfaces.
- Interoperability Issues: Challenges in data sharing across healthcare entities hinder seamless care coordination and communication.
Addressing EHR Challenges
To overcome these challenges, healthcare organizations and software developers can implement various strategies, including:
- Prioritizing user experience and simplicity in EHR design
- Integrating clinically relevant features, such as e-prescribing and mobile access
- Fostering interoperability to facilitate seamless data exchange
- Providing comprehensive training and support for EHR users
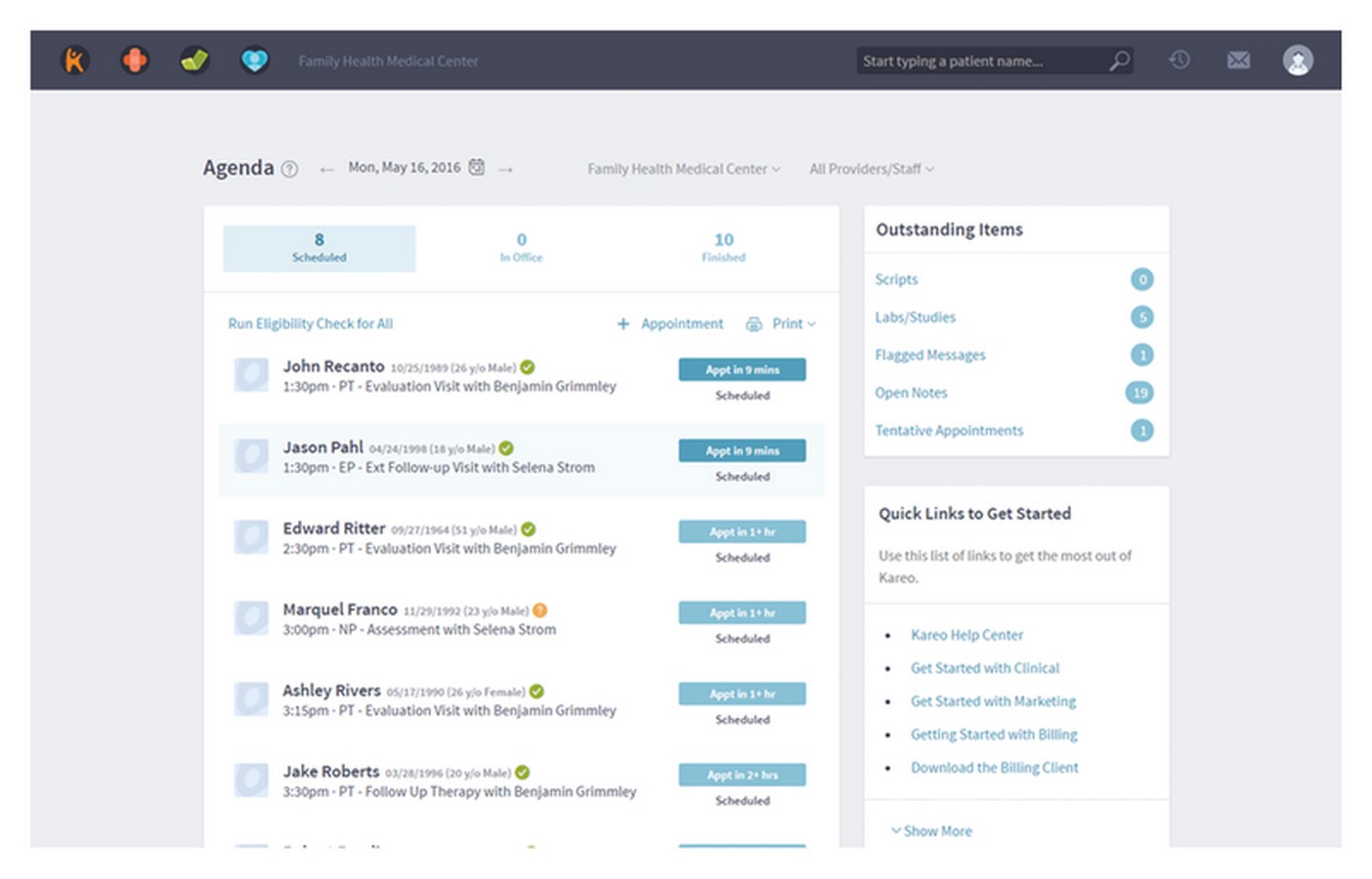
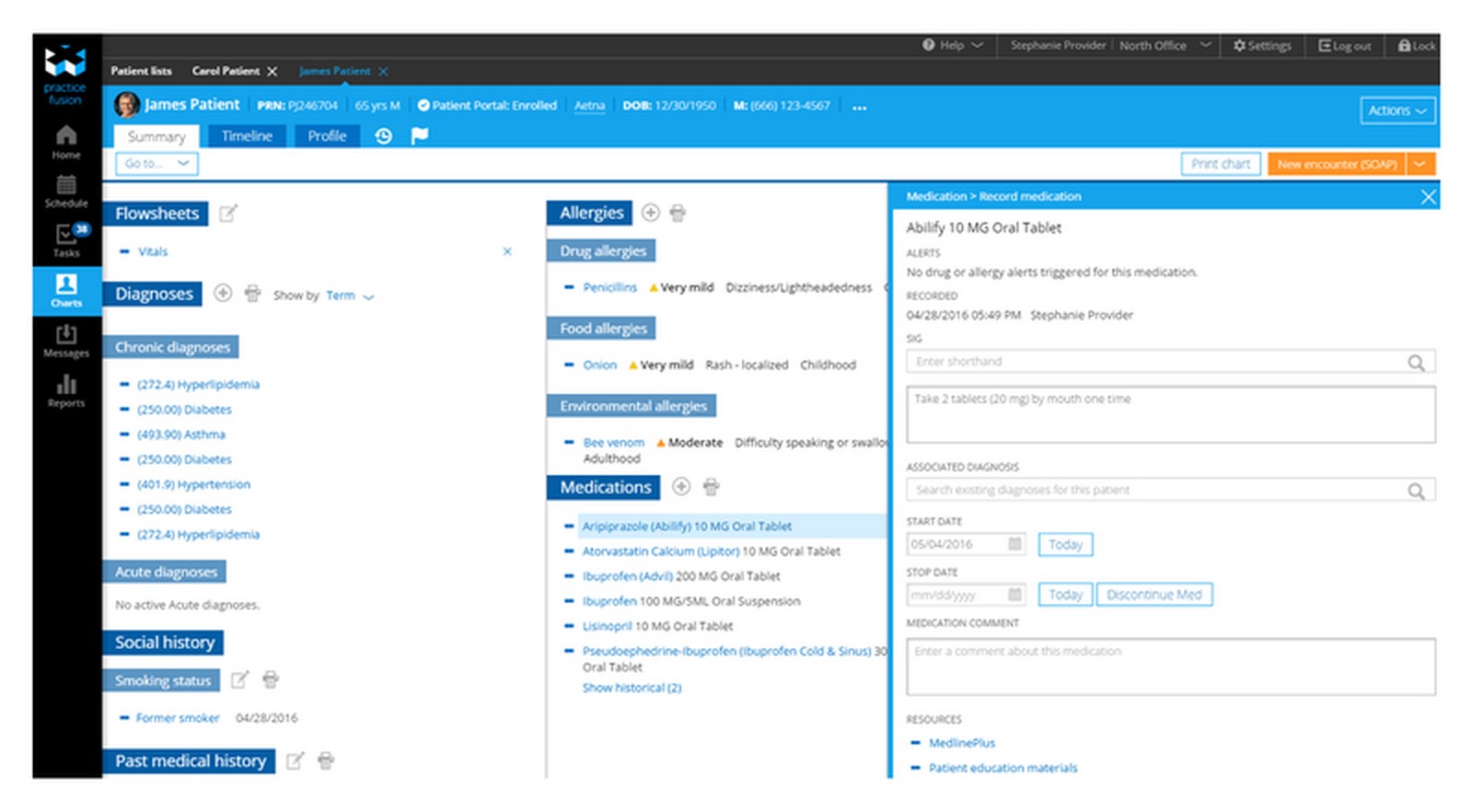
Examples of Leading EHR Software
Examining successful EHR vendors, such as NextGen Healthcare and Kareo, offers valuable insights into key features and functionalities. These vendors demonstrate the importance of robust data sharing, patient engagement tools, and user-friendly interfaces in EHR systems.
Conclusion: Building a Better Healthcare Experience
In conclusion, EHR systems play a crucial role in modernizing healthcare delivery, offering benefits such as improved efficiency and patient outcomes. By addressing the challenges and leveraging best practices in EHR development, healthcare organizations can create systems that empower providers, engage patients, and ultimately enhance the quality of care.